Case Report: Lethargy?
Our latest case report from Dr. Brady Pregerson. Do you know the appropriate diagnosis?
History: A 72-year-old male with a history of lung cancer presents to the emergency department for 3 days of progressive lethargy and an episode of vomiting today. He denies syncope, palpitations, diarrhea, abdominal pain, SOB, fever, cough or other complaints.
Exam: Vital signs show a BP of 82/51 and a pulse of 144. He is ill appearing. Abdomen is diffusely tender but without guarding
Initial differential diagnosis: Tachydysrhythmia, electrolyte abnormality, abdominal catastrophe, sepsis
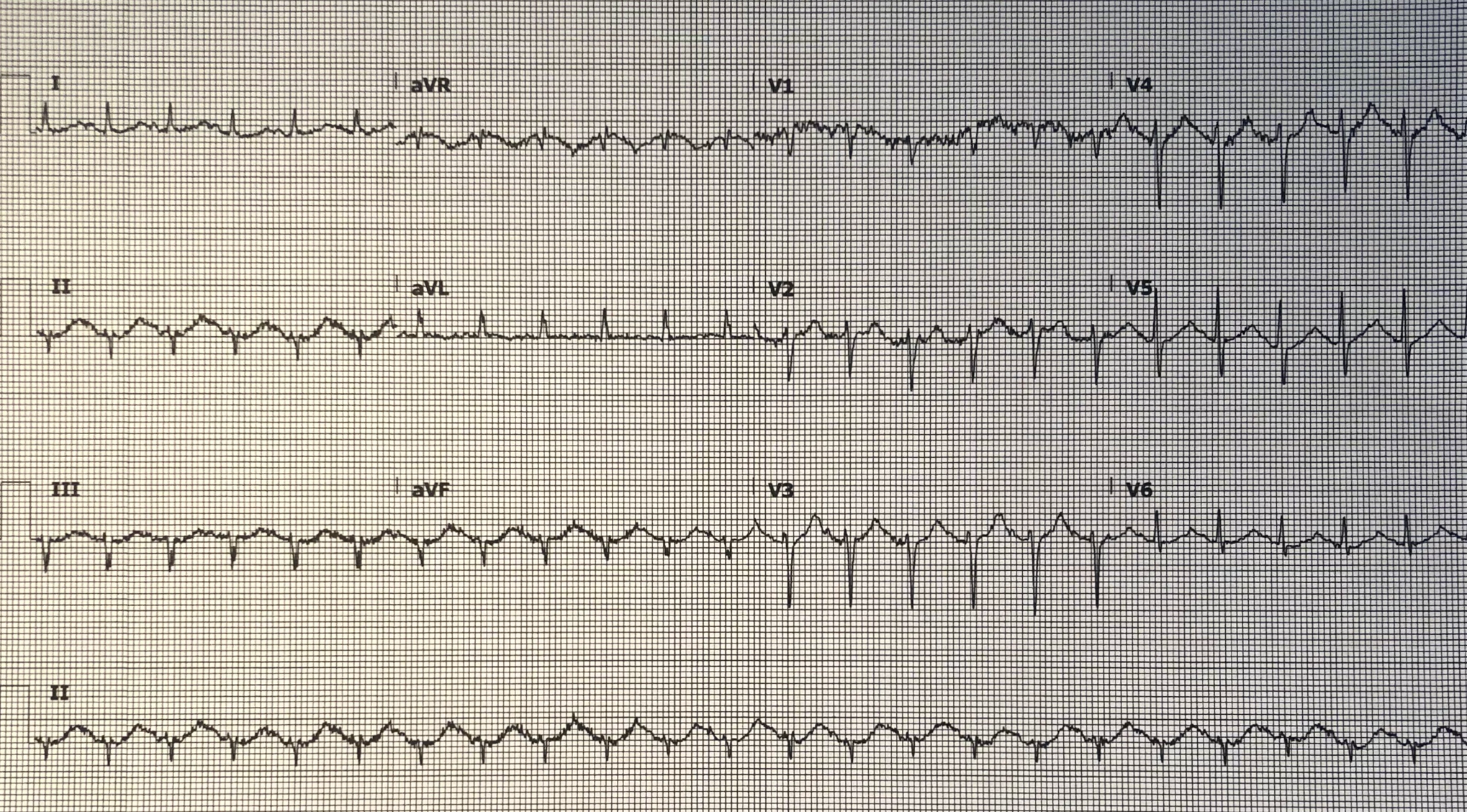
Initial EKG:
COMPUTER EKG READ:
Tachycardia
Ectopic atrial rhythm
Do you agree with the computer? What should you do next?
EKG ANALYSIS, CASE OUTCOME & 1-MINUTE CONSULT:
EKG analysis (peer-reviewed by Dr. Stephen W. Smith of Dr. Smith’s ECG Blog): The computer read is incorrect; it calls the rhythm incorrectly and misses the long QT interval. There are P waves – they are just small and somewhat obscured by artifact and by their location within the terminal part of the T wave as a result of both a long QT interval and severe tachycardia. Nevertheless, P waves can be seen decently well in leads I & V6. Many computers misinterpret a sinus rhythm as something else because they only analyze for P waves in lead II, ignoring other leads. The cardiologist who overread this EKG was also fooled and read the rhythm as atrial flutter. To confirm the rhythm and evaluate for possible SVT, adenosine was given; this caused the pulse to drop to about 110 and P waves were more clearly visible. Lewis leads could have been tried instead or in addition if needed for further clarification. The patient’s initial EKG is suggestive of hypokalemia in multiple ways as follows: sagging ST segments, a very long QT or QU interval with U-waves and T-wave morphology that has a “rooftop” morphology. The rooftop shape of the T wave is due to a U-wave following immediately after the peak of the T-wave and is typically not seen unless the potassium is 3.1 or lower.
Case Conclusion: The potassium was almost normal at 3.4 and the magnesium was normal, however the pH was 6.9 so the potassium would be significantly lower had the pH been corrected (pH down by 0.1, increase in K+ by 0.6). Perhaps this offers a possible explanation of the significant EKG changes. On CT the patient had a perforated colon from metastatic disease. He went to the OR and survived.
Source: The Emergency Medicine 1-Minute Consult Pocketbook
Case Lessons:
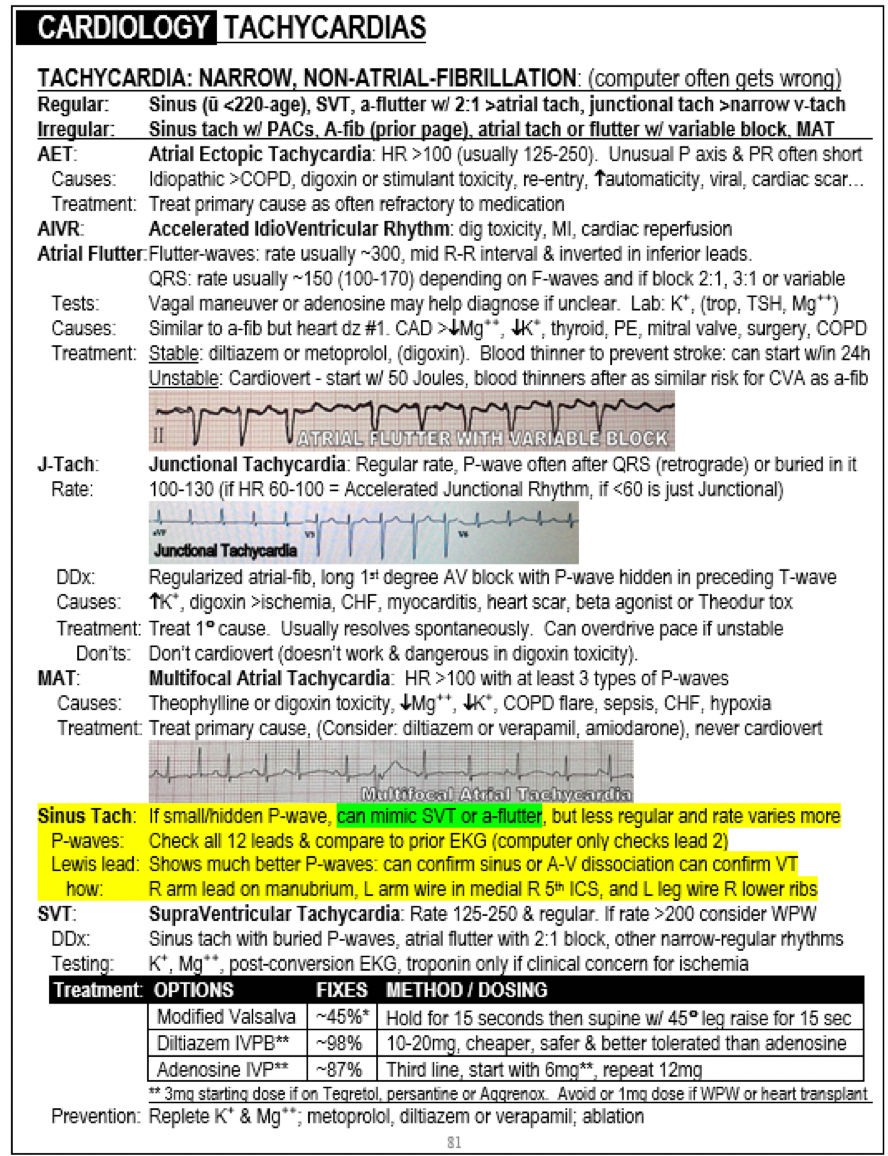
1. The computer not infrequently misreads the rhythm, especially when there is a small P-wave, tachycardia, a long QT interval and/or artifact as each of these can each obscure the P-wave. Sinus tach if fast enough can look like SVT or atrial flutter. If there are PAC’s that make the rhythm more irregular, sinus tach even can mimic a-fib.
2. Long QT can be caused by medical conditions and medications but always check first for low potassium, magnesium or calcium.