Bradycardia, But Why?
An 87-year-old man with a history of mild dementia on Aricept and hypertension on benazepril is brought to the emergency department by family after a possible fall.
Figure 1. Please click here to enlarge
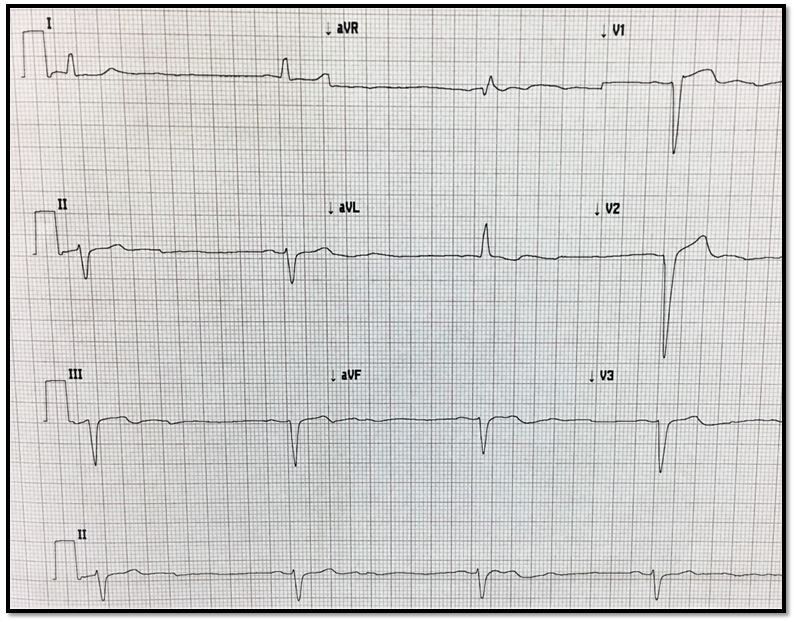
Figure 2. Please click to enlarge
History
An 87-year-old man with a history of mild dementia on Aricept and hypertension on benazepril is brought to the emergency department by family after a possible fall. His daughter came to visit and found him sitting up against a wall in his bedroom and thinks he may have fallen, but saw no injuries. She says that has seemed more tired and more forgetful than normal over the past week and it has been getting progressively worse. It wasn’t that noticeable until today, so she had just been keeping tabs on him, but now she wants him checked out.
The patient and the daughter both deny that there has been any fever, vomiting, pain, trouble breathing, or other complaints. The daughter says that he lives alone and has been able to continue managing his affairs with only minimal outside help. Other than the medications listed above he is only taking vitamins and occasional Pepcid for acid reflux.
Examination
The patient’s vital signs were all normal with a pulse in the 60s. However, while you are in the room you notice that the heart rate on the cardiac monitor occasionally drops for 5-10 seconds down into the 40s and even the 30s.
The patient seems to be a bit lethargic but follows command. The rest of his physical exam is otherwise unremarkable except for his memory being 2 out of 3 items at 2 minutes.
Initial Concerns:
• UTI
• Head injury
• Heart block
Testing:
• Blood and urine unremarkable
• CT head normal
• ECG – see tracing in Figure 1 at right (please click to enlarge)
Questions1. What does the ECG tracing show?
2. What should you do next?
Please click below for answers and discussion.
Answers
1. What does the ECG tracing show? The ECG tracing shows sinus bradycardia at a rate of ~32 beats/min.
2.What should you do next? Search for a cause of the delirium and bradycardia and if none are found, hold any medications that could cause either.
Discussion
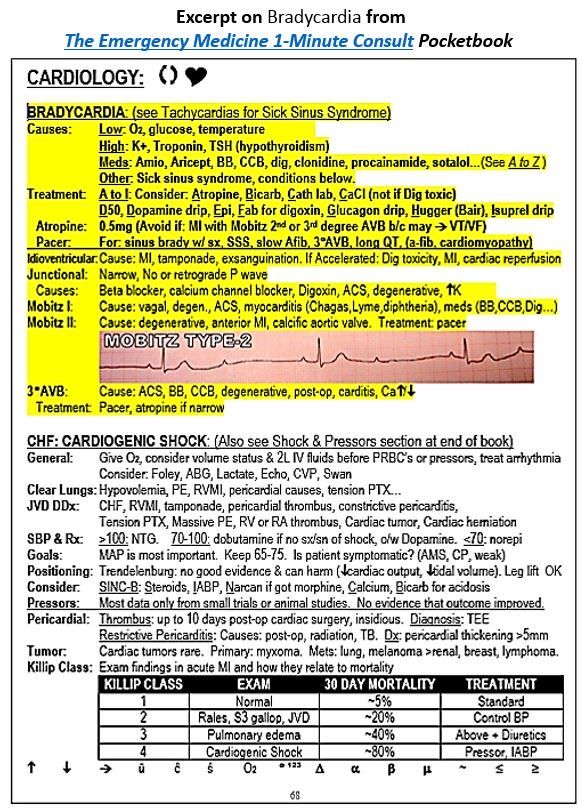
Bradycardia has a plethora of causes, many of which can also cause altered mental status. In addition, bradycardia can itself cause delirium if the blood pressure drops. Many of the causes of bradycardia are listed at the top of the highlighted section of the page shot in Figure 2 at right. Some of the more immediate life-threatening causes include heart block, hypothermia, hypoxia, hyperkalemia, and hypoglycemia. Some of the more common causes of bradycardia include heart block and medications, especially beta-blockers.
Before blaming a medication for bradycardia, a search for another or additional causes should be made. If this search is negative, any suspect medications should be held and the patient monitored for improvement over 1-2 half-lives. This patient was not on any of the medications in the list at right except for Aricept, which is an oral procholinergic agent with a long half-life that is often prescribed in Alzheimer disease. Bradycardia is an uncommon but known side effect of procholinergic agents like Aricept. More common side effects may include headache, nausea, and diarrhea, while other uncommon side effects include hypotension and chest pain.
Case conclusion
No obvious medical cause for the bradycardia or delirium were discovered. The patient was not taking any medications known to cause bradycardia other than Aricept. Aricept was held and he was admitted for observation. His symptoms gradually improved over a few days and he was discharged. The half-life of Aricept is days.