Hypomagnesemia in an 89-year-old Woman
The most common cause of hypomagnesemia is a diuretic; it may be present even when potassium level is normal.
An 89-year-old woman with a history of hypertension presents to the ED with one day of severe pleuritic left-sided chest pain radiating to her back, palpitations, and left-sided twitching. She denies, syncope, dyspnea, fever, or history of any of these events in the past. She takes 3 medications for her hypertension.
On physical examination she is screaming in pain, begging for pain medicine. Vital signs are normal except for a blood pressure of 172/75 mm Hg with similar blood pressure in both arms. The rest of her exam is normal except for an irregular heart rhythm and mild twitching of the left arm.
Her ECG is shown in Figure 1, below. The computer ECG read is: atrial fibrillation with ST and marked T-wave abnormality.
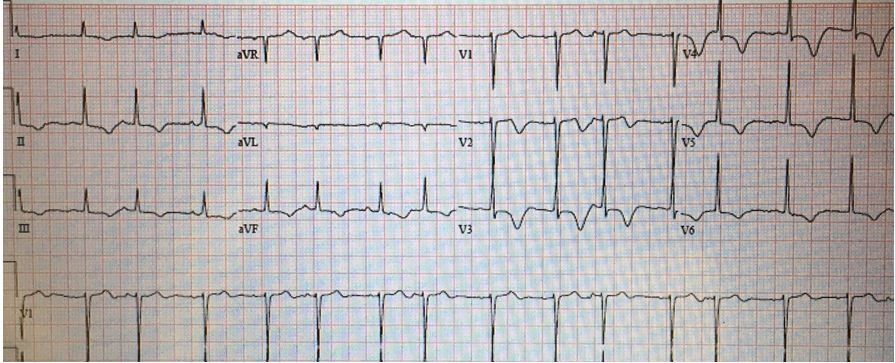
Figure 1. Initial ECG tracing. What’s your ECG read?
Some of the QRS complexes appear to have P waves and others do not making it unlikely that this is atrial fibrillation but rather sinus rhythm with frequent PACs. Multifocal atrial tachycardia could also be considered as there appears to be some variation in the P waves.
What’s in your differential diagnosis?
With severe chest pain that is associated with ST-T wave changes, ischemia definitely needs to be considered. Since the chest pain radiates to the back and there are concomitant CNS concerns, aortic dissection should also be emergently ruled out. An acute neurologic process such as stroke or seizure may additionally manifest on ECG with marked ST-T changes and a prolonged QT interval. Electrolyte abnormalities should also be considered, especially considering that the QT interval appears prolonged and the patient may be having a seizure.
Discussion
This patient’s presentation was quite confusing. Because of the impressive ECG changes and severe chest pain radiating to the back, cardiology was paged and a CT of the chest ordered to rule out aortic dissections. The CT was negative for dissection and PE as well. Results of a nuclear stress test also were negative. The cause of this patient’s chest pain was never determined. After CT she developed a generalized seizure which resolved with benzodiazepines. A brain MRI was negative but an EEG was positive. Based on the presence of a prolonged QT interval a serum magnesium level was ordered even though her potassium level was normal. The magnesium level measured low, at 1.1 mEq/L, most likely a side effect of the hydrochlorothiazide she was taking for her hypertension. After IV magnesium repletion a repeat ECG was performed; the tracing is shown in Figure 2. The QT interval has normalized as have the ST and T-wave changes. Now instead of PACs she is having PVCs.
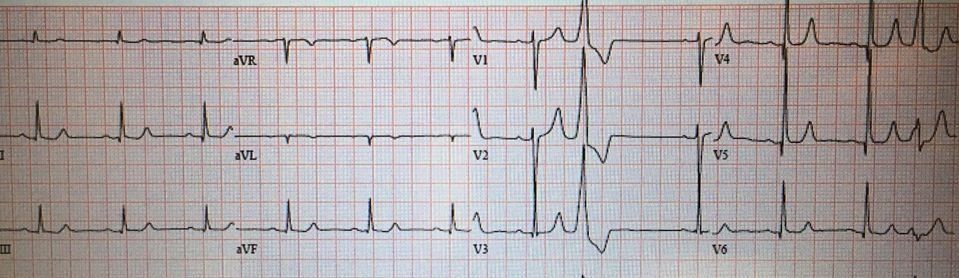
Figure 2. ECG tracing after magnesium repletion. Hypomagnesemia is often asymptomatic but paresthesia and tremors may occur. For other symptoms see the Table below. The most common cause of hypomagnesemia is a diuretic. Other frequent causes are also covered in the Table. Hypomagnesemia may cause both ECG and neurologic changes, as seen in this patient. ECG changes may include flat or inverted T-waves and QT interval prolongation. In addition, both ventricular and supraventricular dysrhythmias such as atrial fibrillation, PACs and PVCs and even ventricular tachycardia may occur. See Table below for more specifics. Treatment is initially with IV magnesium, which may be followed by a change in medication, in this case the diuretic HCTZ, by treating the underlying cause and/or initiating an oral magnesium regimen such as magnesium-oxide.
Table
For additional at-a-glance information, click on images below.