Case Report: Congestive Heart Failure?
A 72-year-old male with a history of ESRD, CHF and DM presents to the hospital with 6 weeks of slowly progressive leg edema and 3 weeks of SOB/DOE that has become much worse over the past 24 hours and is associated with a new cough. What's your diagnosis?
CASE REPORT: Congestive Heart Failure?
History: A 72-year-old male with a history of ESRD, CHF and DM presents to the hospital with 6 weeks of slowly progressive leg edema and 3 weeks of SOB/DOE that has become much worse over the past 24 hours and is associated with a new cough. He denies syncope, palpitations, chest pain, fever, or other complaints.
Exam: Vital signs are normal except for a pulse-ox of 91% on room air and a RR of 30. Breath sounds are diminished but symmetric, and legs have symmetric pitting edema without erythema. His physical exam is otherwise normal.
Initial differential diagnosis: CHF, Pulmonary Embolism, Acute Coronary Syndrome, Pneumonia
Initial EKG:
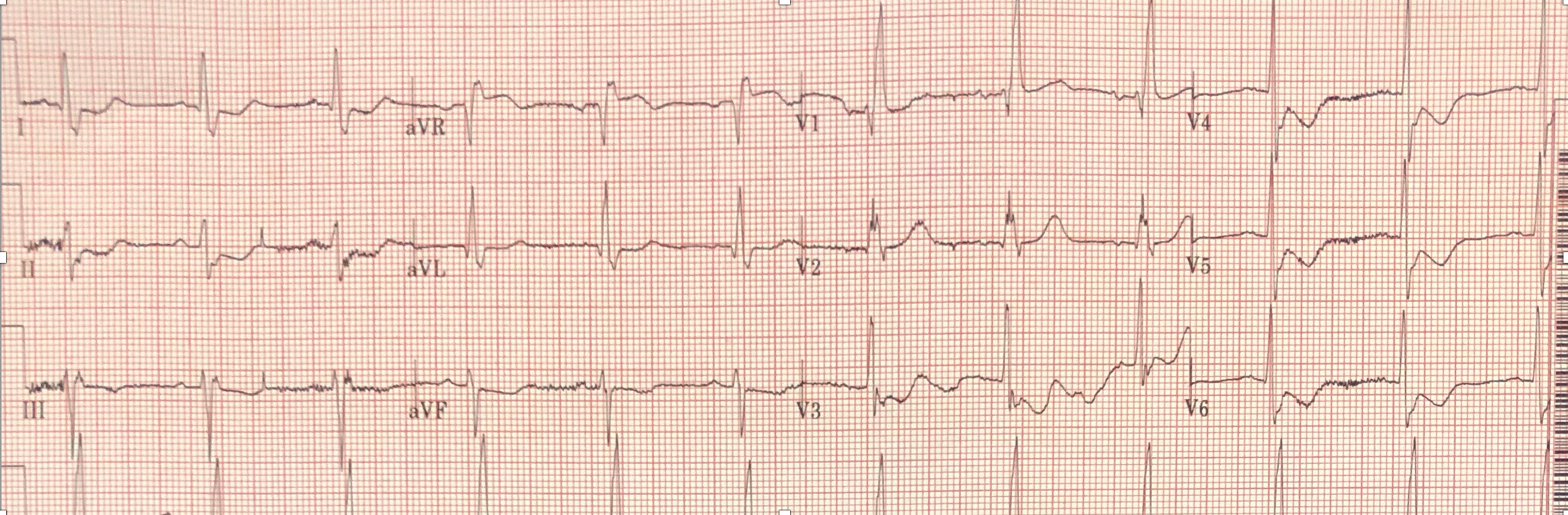
COMPUTER EKG READ:
- Normal sinus rhythm
- Right bundle branch block
- Left anterior fascicular block
- Bifascicular block
- T wave abnormality, consider inferolaeral ischemia
Do you agree with the computer? What should you do next?
EKG ANALYSIS, CASE OUTCOME, 1-MINUTE CONSULT & CASE LESSONS:
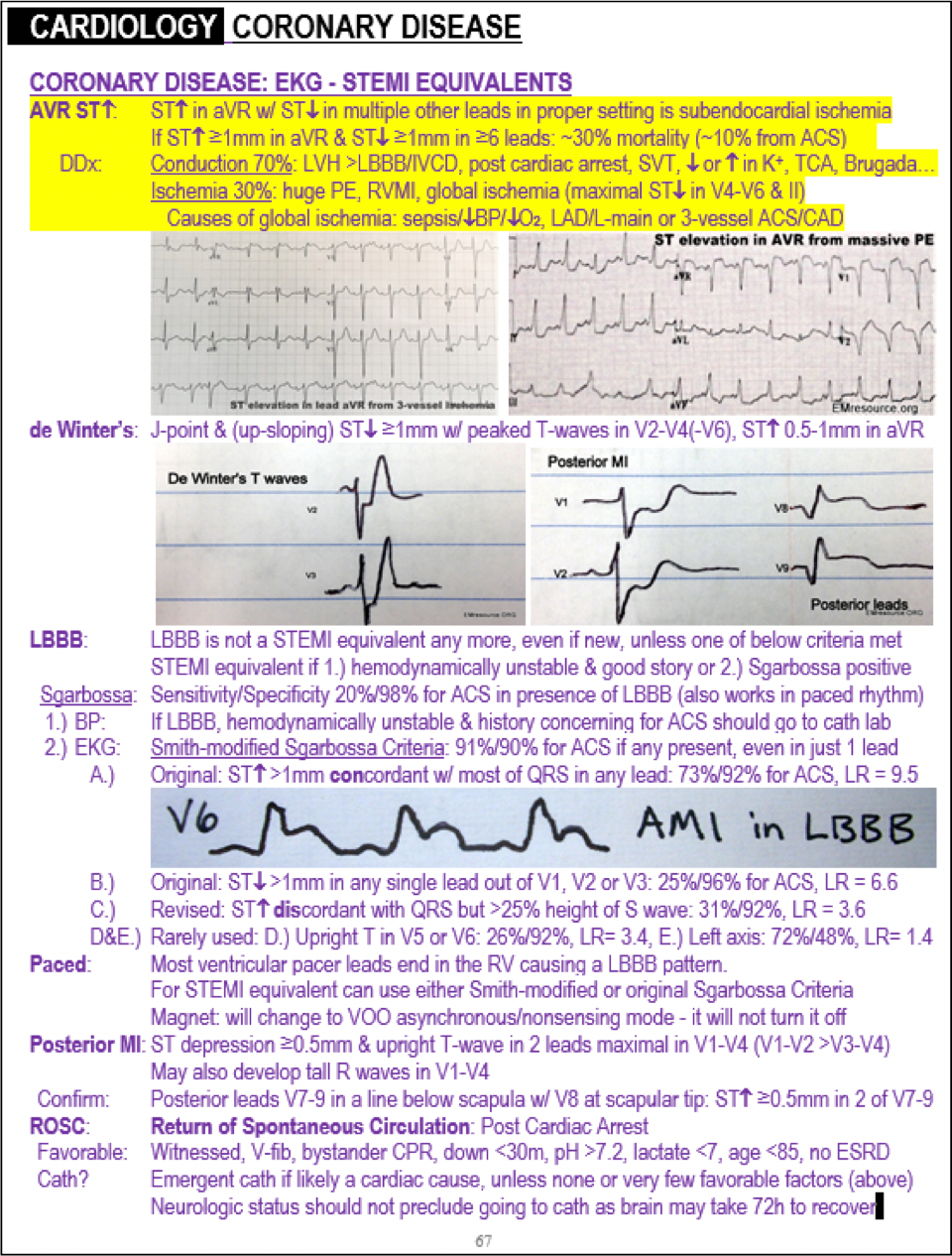
EKG analysis (peer reviewed by Dr. Stephen W. Smith of Dr. Smith’s ECG Blog): The computer read is correct but incomplete. There is ST elevation in aVR with semi-diffuse ST depression that is not caused by the RBBB. These EKG findings are concerning for subendocardial ischemia due to an incomplete coronary occlusion with insufficient flow to perfuse the entire myocardial wall. Since the subendocardium is more vulnerable to ischemia due to pressures within the myocardium, it can become ischemic even without complete occlusion. This causes ST depression in overlying leads with reciprocal ST elevation in aVR. In the proper clinical setting, this calls for urgent catheterization even though the occlusion is not complete because 1) there is ongoing ischemia and myocardial damage and 2) the partial occlusion can progress to complete occlusion if left untreated.
Case Outcome: Initial troponin was 8.0 (99% URL <0.030: troponin-i immunoassay, Abbott laboratories). Cardiology was consulted and the patient went to cath urgently. Repeat troponin a few hours after the first was 10.9. At cath, there was an 80% LAD occlusion that was stented.
aVR ST elevation fromThe Emergency Medicine 1-Minute Consult:
Source: The Emergency Medicine 1-Minute Consult Pocketbook
Case Lessons
- ST elevation in aVR has many possible causes, one being reciprocal change to ST depression in left-sided leads as part of non-occlusive ACS causing subendocardial ischemia.
- Always look for a reason when someone's condition has become worse in the past 24 hours. This patient initially seemed like routine CHF but his acute worsening was due to acute ischemia.