Antiplatelet and Anticoagulant Therapy Varies Greatly After TAVR
A review published in JAMA Cardiology reports that while patients with severe aortic stenosis are increasingly undergoing transcatheter aortic valve replacement (TAVR) procedures in place of surgery, there is little evidence on how best to utilize adjunctive antithrombotic therapy after the treatment.
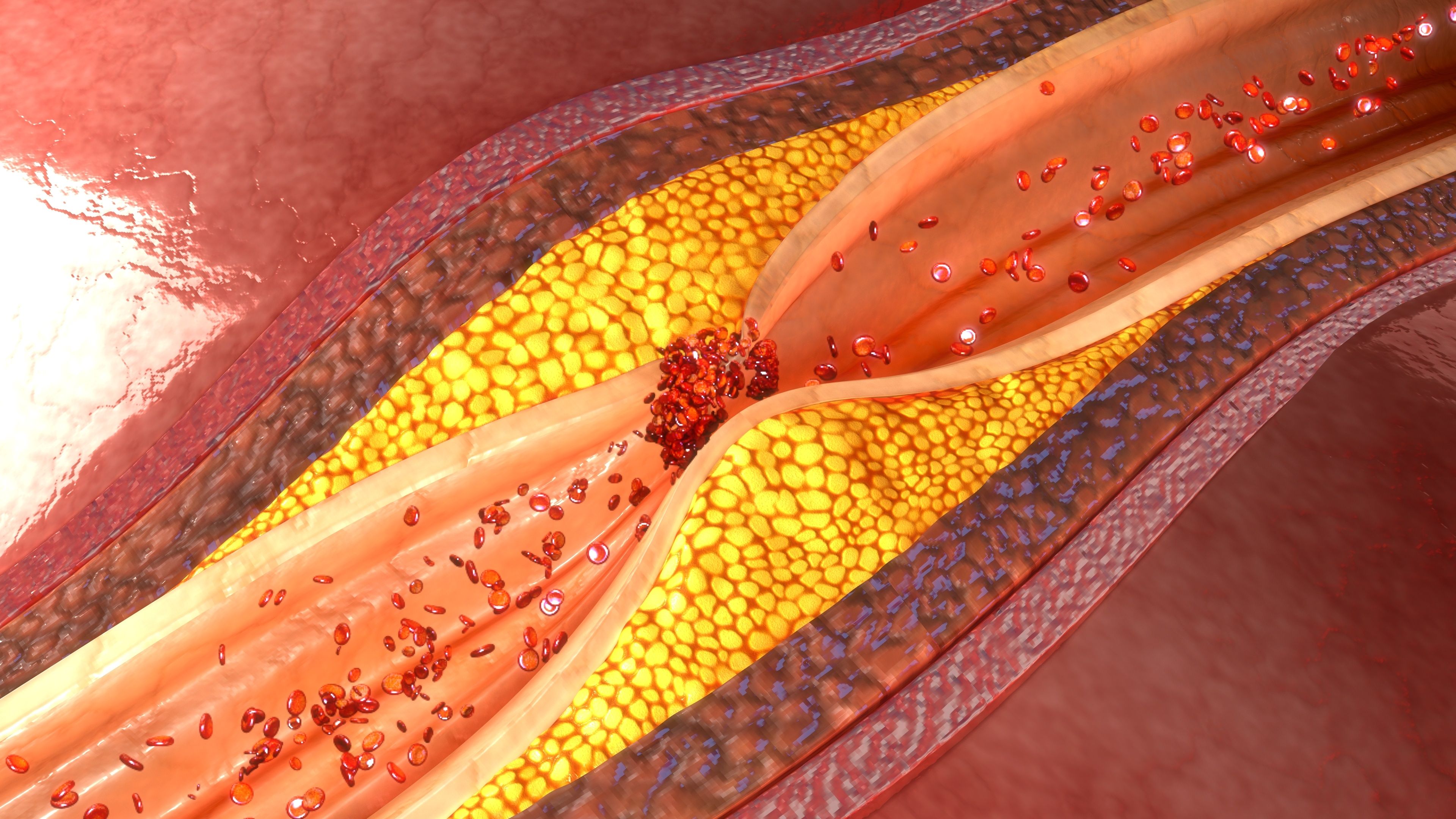
(©7ActiveStudio, AdobeStock)
A review published in JAMA Cardiology reports that while patients with severe aortic stenosis are increasingly undergoing transcatheter aortic valve replacement (TAVR) procedures in place of surgery, there is little evidence on how best to utilize adjunctive antithrombotic therapy after the treatment.
The procedure is increasingly being conducted in more patients. It is considered less invasive, but the risks of ischemic and bleeding complications are considerable. For example, even though stroke risk are lower, they can still occur. At one-year post-op, life-threatening or major bleeding events, and ischemic stroke events, occur in approximately 10 percent of patients.
Recent clinical trials show that it is associated with lower stroke risk as compared to cases in which patients have had valve replacements surgically, still, the risk for stroke at the time of the procedure is high and it accrues over time. Treatment guidelines recommend the use of dual antiplatelet therapy for three-six months after the procedure, but Yuichi Saito, M.D., writes in JAMA Cardiology that there is little evidence to support this treatment modality. To date, there are no risk prediction models to guide treatment decisions for antithrombotic therapy.
"In patients with no indication for oral anticoagulation, current registry-based evidence suggests that single antiplatelet therapy may be safer than dual antiplatelet therapy. Similarly, oral anticoagulation monotherapy appears superior to anticoagulation plus antiplatelet therapy in those where oral anticoagulant use is indicated," Dr. Saito and colleagues wrote.
Adjunctive antithrombotic therapy is used to mitigate thrombotic risks in patients undergoing transcatheter aortic valve replacement, but there can be bleeding complications, researchers wrote. At least half of bleeding and cerebrovascular events occur within 30 days of the procedure.
Although treatment guidelines recommend antithrombotic regimens after the procedure, there is little evidence to guide this decision. And, as a result, there is great variation in how physicians prescribe this treatment.
"Although the use of dual antiplatelet therapy for three-six months after TAVR is the guideline-recommended regimen, this practice is not well supported by current evidence. In patients with no indication for an oral anticoagulation, single antiplatelet therapy may be safer rather than dual antiplatelet therapy. Similarly, oral anticoagulation monotherapy might be superior to an oral anticoagulation plus single antiplatelet therapy in patients with an oral anticoagulation indication. To date, no risk prediction models have been established to guide antithrombotic therapy. Ongoing investigations will provide better guidance for adjunctive antithrombotic regimens for patients with aortic stenosis undergoing TAVR," researchers wrote.
REFERENCE
Yuichi Saito, M; Tamim Nazif, MD; Andreas Baumbach, MD1; et al. "Adjunctive Antithrombotic Therapy for Patients With Aortic Stenosis Undergoing Transcatheter Aortic Valve Replacement." JAMA Cardiology. Published online November 13, 2019. DOI:https://doi.org/10.1001/jamacardio.2019.4367